Some call it “framing” the
conversation a certain way that heightens the odds of a particular response. No matter what the
procedure is called, end-of-life decisions about treatment options for
critically and terminally ill patients can be influenced greatly by how doctors
present information to patients and caregivers.
In a study about doctors’end-of-life language, a simulation involving an
older adult with end-stage cancer and life-threatening hypoxia (deficiency of oxygen reaching the tissues ) was followed by a debriefing interview. Doctors
participating were hospitalist, emergency medicine, and critical care
physicians from three academic medical centers. Their encounters regarding
presentation of treatment options were observed in real time and analysed.
Results:
1) Among 114 physician
subjects, 106 discussed life-sustaining treatment, 86 discussed palliative care,
and 84 discussed both.
2) Doctors framed life-sustaining
care as necessary (53%), while framing palliative care as optional (49%).
3) Among doctors who
framed life-sustaining care as imperative, 16 (30%) felt intubation (insertion
of a tube through mouth and airway to assist with patient’s ventilator
breathing) would be inappropriate in this clinical situation.
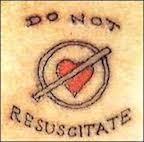
The majority of doctors framed end-of-life patient
options by implying
that life-sustaining treatment was the expected or preferred
choice.
Framing options in this way can greatly influence treatment decisions
made by patients and caregivers.
The following video is an excerpt of a
televised edition of Frontline. It
features patients, families, and doctors facing complicated end-of-life
decisions at the Mount Sinai Hospital intensive care unit in New York City:
Frances Shani Parker, Author
Becoming Dead Right: A Hospice Volunteer
in Urban Nursing Homes is available in paperback and e-book
editions in America and other countries at online and offline booksellers.